COVID-19: How do different vaccines work?
04 February 2021
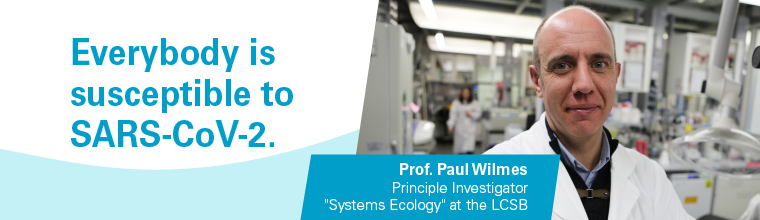
How do different vaccines work? And why are people reacting differently to them? These are questions we asked Prof. Paul Wilmes, microbiologist at the Luxembourg Centre for Systems Biomedicine. As a spokesperson of the Research Luxembourg COVID-19 Task Force, he follows the development of the pandemic very closely. In this interview, he provides insights on the current status of the COVID-19 vaccines.
This article was originally published by the University of Luxembourg
Can you give us an overview which COVID-19 vaccines are currently available?
In Luxembourg, there are currently two vaccines against COVID-19 available, one from Pfizer/BioNTech and one developed by Moderna. Another vaccine from AstraZeneca has been approved by the European Medicines Agency (EMA). However, there are others being tested in clinical trials at the moment, so we can expect additional COVID-19 vaccines to become available during the year.
There is also ‘Sputnik-V’, the vaccine developed in Russia, but this has so far not been approved by the EMA. Likewise, China developed a vaccine, but recent data show that this vaccine has a quite low efficiency of only around 50%, in contrast to more than 94% for the vaccines by Pfizer/BioNTech and Moderna.
What is the difference between these vaccines?
Apart from the differences in efficacy, there are different underlying mechanisms in how the vaccines work. The Chinese vaccine uses inactivated viral particles to evoke an immune response which is a classical approach still used in vaccinations against rabies and polio, but also often results in more side-effects.
Another way is to use another virus as a carrier, for example an adenovirus, to deliver parts of the genetic material of SARS-CoV-2 into the cells. This has become a standard approach for many vaccines in the past. The COVID-19 vaccines from Russia and from AstraZeneca use this approach.
A new approach which has been in development over the past decade involves bypassing the carrier-virus and injecting directly parts of the SARS-CoV-2 genetic information in the form of mRNA. A great advantage of this technology are the comparably low production costs and easy adaptability of the vaccine in the case that the virus mutates and escapes the vaccine.
The type of vaccine also determines how many doses one needs to receive in total. The currently approved vaccines require a second dose after a few weeks to achieve an optimal effect. Some vaccines which are now in the final stages of clinical development need to be administered only once to acquire immunity, which will hopefully simplify the logistics of vaccination procedures in the future.
What happens in the cells when you get vaccinated?
Generally speaking, vaccination is an artificial way of exposing your immune system to key molecules from a pathogen against which you want to build up immunity. The immune system recognises specific protein parts of the virus which are called antigens. Such antigens can either be introduced directly during the vaccination process or by using their genetic information such as mRNA to produce the antigen within cells. However, it is important to note that only a very small part of the virus’ genetic information is brought into one’s own cells upon vaccination. It is not possible to create a virus out of these fragments and thus vaccination cannot induce the corresponding disease.
In either case, the antigen produced by the human body is then literally presented on the surface of the muscle cells around the injection site. This then triggers the immune system as the antigen is recognised as being foreign to the body.
Why do people react differently to vaccinations and why is it not 100% efficient?
Although the principal mechanism of action of a vaccine is defined, the responses in different individuals might be different. In some people, the immune system might not recognize the presented antigen as a foreign particle, and thus not raise an immune response towards it. Also, the production rate of the antigen in the cells might be lower in some people and thus not enough of it might be available to trigger the immune system.
The individual’s prior exposure to other viruses also can play a role: the immune system could potentially identify this as a viral antigen easier if the person was infected with another closely related coronavirus in the past as for instance those causing the common cold. We now know that there is some cross reactivity between different coronaviruses in terms of our immune response, so people having developed antibodies against other coronaviruses may have a different response towards SARS-CoV-2.
Yet, it is important to keep in mind that in principle everybody is susceptible to be infected by the SARS-CoV-2 virus as humankind has not been exposed to it throughout evolution. As a consequence, there is no specific and efficient immune response by default.
Is there enough vaccine available for everybody? How long will it presumably take for everyone in Luxembourg to receive the vaccination?
At the moment, there are two major bottlenecks: one is the production of the vaccine in itself and the other concerns the logistics of administration.
The manufacturers are constantly upscaling their production and also new vaccines are expected to be approved in the near future, yet at the moment the number of doses promised have not been met.
Nevertheless, to ensure an efficient vaccination procedure for everybody in Luxembourg, national vaccination centres have been opened. One of the mRNA vaccines requires storage and transport at extremely cold temperatures of -80 °C which makes the logistical efforts quite challenging and thus requires centralisation.
The European Union has negotiated the number of doses to be received from the manufacturers to distribute them equally among their member states according to population size. Thus, the absolute number of doses available in Luxembourg is lower compared to countries such as France or Germany. According to the Joint Purchasing Agreement, Luxembourg will receive 0.14% of the doses ordered by the EU, which is also the proportion of Luxemburg citizens in the EU. While this sounds low, there is a good chance to offer the vaccination to everybody in Luxembourg until the end of 2021, as far as we can tell now. However, what remains absolutely crucial is that as many people as possible will get vaccinated as fast as possible to get out of the pandemic.
What are the priority groups for vaccination and who decides when people are invited to get vaccinated?
The Luxembourg Government has decided to give the highest priority to individuals with the highest risk to be exposed to the virus and infect others or to develop a severe course of COVID-19 upon infection. This includes for example healthcare professionals in key positions as well as older age individuals or those with specific pre-existing conditions which increases the likelihood of severe medical complications linked to COVID-19. The reason behind this strategy is to minimise the number of deaths while at the same time ensuring a functioning healthcare system.
In the end, the authorities will decide when the next group of people is invited to the vaccination centre. The Government’s vaccination strategy is informed by the recommendations of the national ethics board. Recently the Government announced phase 2 of the vaccination strategy in which people over 75 years of age and those particularly vulnerable to the disease because of existing pre-conditions will be vaccinated.